
Show Notes 19 May 2023
This week it’s all about four medical miracles!
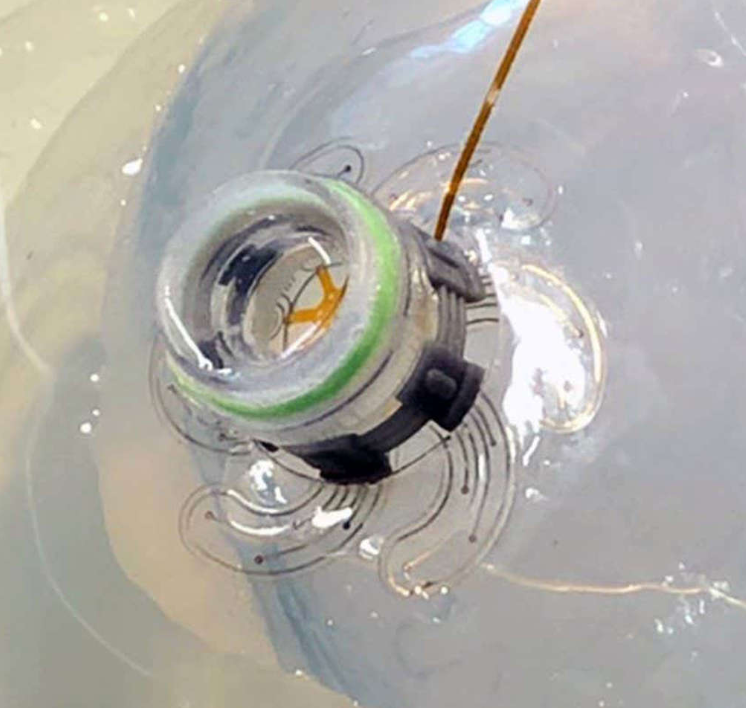
Story 1: Tiny robot injected in the skull spreads its tentacles to monitor the brain
Source: NewScientist Story by Jeremy Hsu
- To fully appreciate the significance of this development we need to set the stage with some background information:
- What we’re going to talk about is an alternative for how electrodes are deployed on the surface of the brain.
- Electrodes that generate electrical impulses to stimulate the brain are used for a variety of purposes, including:
- control abnormal brain activity
- or adjust for the chemical imbalances within the brain that cause various conditions.
- Inserting electrodes is typically done by opening an invasive “hole” in the skull, through which electrodes, or leads, can be inserted.
- With that said, here’s the big news:
- To offer a much less invasive alternative scientists at the Federal Polytechnic School in Switzerland have developed a miniature soft robot that can be inserted through a tiny hole in the skull.
- Once inserted the tiny bot can deploy six sensor-filled legs on the surface of the brain. And these legs can be deployed within the very limited space between the skull and brain [that’s only a 1-millimeter gap].
- A version of this soft robot has been successfully tested in a miniature pig and could be scaled up for human testing in the future.
- The researchers designed the robot’s legs to gently expand to avoid putting too much pressure on the brain.
- Strain sensors embedded in each leg convey information about when the robot legs are fully deployed, without the need for additional cameras or external sensors.
- A strain sensor measures the relative change in length of a component or structure under stress.
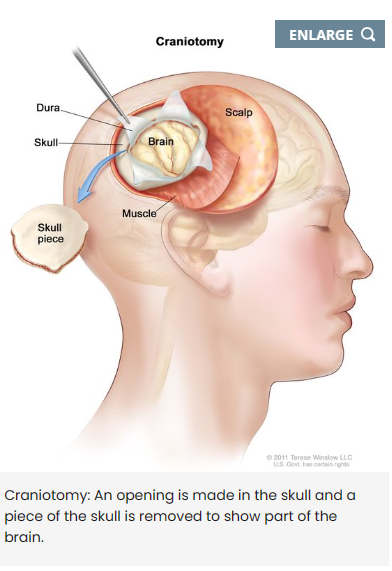
- One of the researchers noted: “There’s actually a really large surface area [on the brain] that you can reach without doing a large craniotomy.”
- Side note: A craniotomy is a major surgery. A surgeon usually considers this type of treatment after diagnosing a brain tumor or life-threatening condition or after a traumatic brain injury. Source: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/craniotomy
- The soft robot is 2 centimeters (0.8 inches) long and its legs are primarily made from flexible silicone polymer. The legs resemble curved flower petals spiraling around the central body of the robot, and when fully extended they cover a diameter of 4 centimeters (1.6 inches). Each leg contains electrodes for monitoring brain activity.
- According to the research team, the legs could be lengthened to 8 or 10 centimeters (3 to 4 inches) in future prototypes without having to increase the size of the hole cut in the skull.
- The robot was tested on a plastic and hydrogel model of the brain. But researchers also showed how they could deploy a straight version of the soft robotic leg – 15 millimeters (0.6 inches) long – on the brain of a minipig.
- In a demonstration inside the live animal, the soft robot’s electrodes recorded brain activity patterns as the researchers electrically stimulated the minipig’s snout.
- Here’s the key takeaway: If this tiny new robot proves safe and effective in humans, it could eventually help monitor and even treat patients who experience epileptic seizures or other neurological disorders.

Story 2: Chemotherapy drug reaches brain in humans for the first time
Source: Northwestern Now Story by Marla Paul
Link:

- A major impediment to treating the deadly brain cancer glioblastoma has been that the most potent chemotherapy drugs can’t permeate the blood-brain barrier to reach an aggressive brain tumor.
- What is the “blood-brain” barrier:
- The blood-brain barrier is a microscopic structure that blocks the vast majority of drugs injected into the circulatory system from reaching the brain.
- The blood-brain barrier is a crucial immunological feature of the human central nervous system. Composed of many cell types, the blood-brain barrier is both a structural and functional roadblock to microorganisms, such as bacteria, fungi, viruses or parasites, that may be circulating in the bloodstream. Source: https://asm.org/Articles/2020/April/How-Pathogens-Penetrate-the-Blood-Brain-Barrier
- Patients with brain cancer cannot be treated with most drugs that are otherwise effective for cancer elsewhere in the body, as these do not cross the blood-brain barrier.
- But now Northwestern University scientists report results of the first in-human clinical trial in which they used a novel, skull-implantable ultrasound device to open the blood-brain barrier and repeatedly permeate large, critical regions of the human brain to deliver intravenously injected chemotherapy drugs.
- This is the first study to successfully quantify the effect of ultrasound-based blood-brain barrier opening to facilitate the deployment of chemotherapy in the human brain.
- Opening the blood-brain barrier [using the new skull-implantable ultrasound device triggered by a sonication process] led to an approximately four- to six-fold increase in drug concentrations in the human brain, the results showed.
- Side note, what is sonication? – Sonication is the act of applying sound energy to agitate particles in a sample, for various purposes such as the extraction of multiple compounds from plants, microalgae and seaweeds. Ultrasonic frequencies are usually used, leading to the process also being known as ultrasonication. Source: https://en.wikipedia.org/wiki/Sonication
- Scientists observed this increase of four- to six-fold increase in drug concentrations in the human brain by experoimenting with two different powerful chemotherapy drugs. To date these drugs have not been used to treat patients with brain cancer because they do not cross the blood-brain barrier in normal circumstances.
- The four-minute procedure to open the blood-brain barrier is performed with the patient awake, and patients go home after a few hours. The results show the treatment is safe and well tolerated, with some patients getting up to six cycles of treatment.
- In addition, this is the first study to describe how quickly the blood-brain barrier closes after sonication. Most of the blood-brain barrier restoration happens in the first 30 to 60 minutes after sonication, the scientists discovered.
- Here’s the key takeaway: The findings will allow optimization of the sequence of drug delivery and ultrasound activation to maximize the drug penetration into the human brain, the researchers said.

Story 3: Scientists Use Electricity to Make Wounds Heal 3x Faster
Source: ScienceAlert.com Story by David Nield
Link: https://www.sciencealert.com/scientists-use-electricity-to-make-wounds-heal-3x-faster
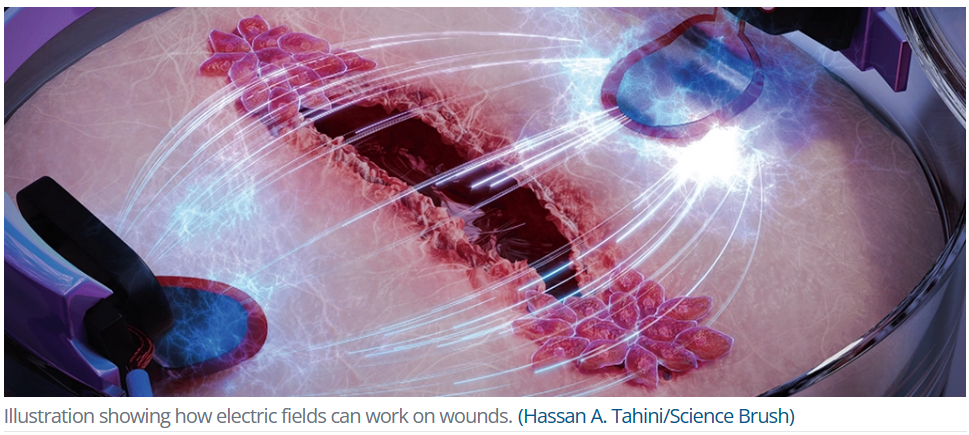
- Scientists have developed a specially engineered biochip that uses electricity to heal wounds up to three times faster than normal.
- It’s well known that electric fields can guide the movements of skin cells, nudging them towards the site of an injury for instance. In fact, the human body generates an electric field that does this naturally. So, researchers from the University of Freiburg in Germany set out to amplify the effect.
- While it might not be used to quickly heal severe injuries, it could radically reduce the time it takes for small tears and lacerations to recover.
- For people with chronic wounds that take a long time to heal, such as in elderly patients, those with diabetes, or people with poor blood circulation, recovering quickly from frequent small, open cuts could be a literal lifesaver.
- While it’s established electricity can assist healing, the impact of an electric field’s strength and direction on the process has never been well established.
- So, the researchers developed a bioelectronic platform and used it to grow artificial skin made up of cells called keratinocytes, which are the most common skin cell type and crucial for the healing process.
- They also compared the application of electric fields on one side of the wound with alternating fields on both sides of the wound.
- Both healthy keratinocytes and keratinocytes designed to resemble those in people with diabetes migrated up to three times faster than skin cells without any electrical interference.
- The team discovered that an electrical push from just one side of the wound proved most effective at repairing the artificial skin in the quickest time. Fortunately, none of the cells were damaged by the electrical fields tested.
- The next stage is testing how all this works on actual wounds in living humans, rather than skin cells grown in the lab.
- Developing practical applications will rely on translating the cheap, readily available used materials in the experiment to real-world situations.

Story 4: Capsule Delivers Electrical Current to Stomach to Stimulate Appetite
Source: Medgadget.com Story by Conn Hastings
Link: https://www.medgadget.com/2023/05/capsule-delivers-electrical-current-to-stomach-for-appetite.html

See video here: https://www.youtube.com/watch?v=Tybn9nbwfZc
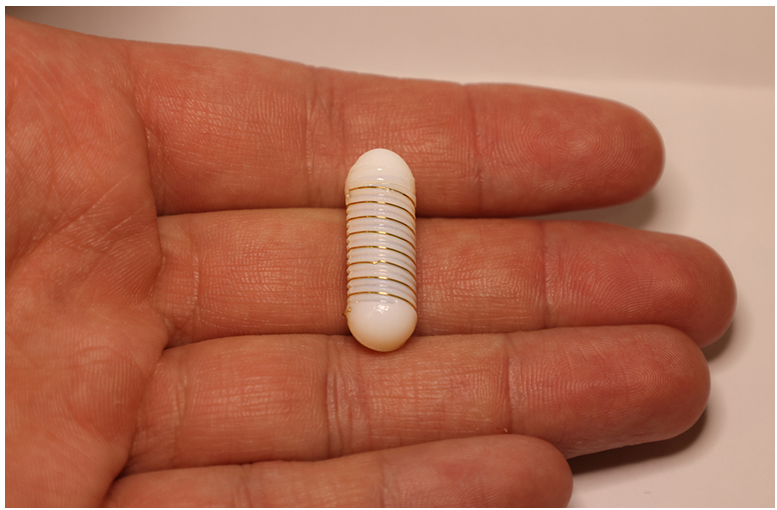
- To help patients with eating disorders or conditions such as a wasting condition that can occur in cancer patients, researchers at MIT have developed an ‘electroceutical’ capsule that is designed to be swallowed and which will deliver a small electrical current to the stomach wall.
- Side note on wasting condition – It is a complex problem. It involves changes in the way your body uses proteins, carbohydrates, and fat. You may also burn up calories faster than usual.
- The electroceutical capsule device contains an external electrode that wraps around its exterior and small grooves that draw liquid away from the electrode and help it to contact the stomach wall.
- The technology stimulates endocrine cells in the stomach lining to secrete more of a hormone called ghrelin, which stimulates appetite and reduces nausea.
- The concept of delivering electricity to the stomach to assist with gastrointestinal issues was first trialed in patients who experience slow gastrointestinal motility, in the hope that it would enhance stomach contractions.
- The MIT team tested their hypothesis in animals, finding that a small electrical current in the stomach did indeed increase levels of the hormone called ghrelin. To translate this into something that had clinical potential, they have now designed the electroceutical capsule small enough to be simply swallowed, avoiding the need for a surgical procedure.
- The MIT team designed the capsule for maximum contact with the stomach wall. Fluids in the stomach could interfere with this, so the capsule contains small grooves with a hydrophilic coating that draws the fluid away from the electrode.
- Hydrophilic means having a tendency to mix with, dissolve in, or be wetted by water.
- Fun fact: The concept was inspired by the skin of the Australian thorny devil lizard, which contains tiny grooves that help to draw water towards the lizard’s mouth.


